What is Post-thrombotic Syndrome?
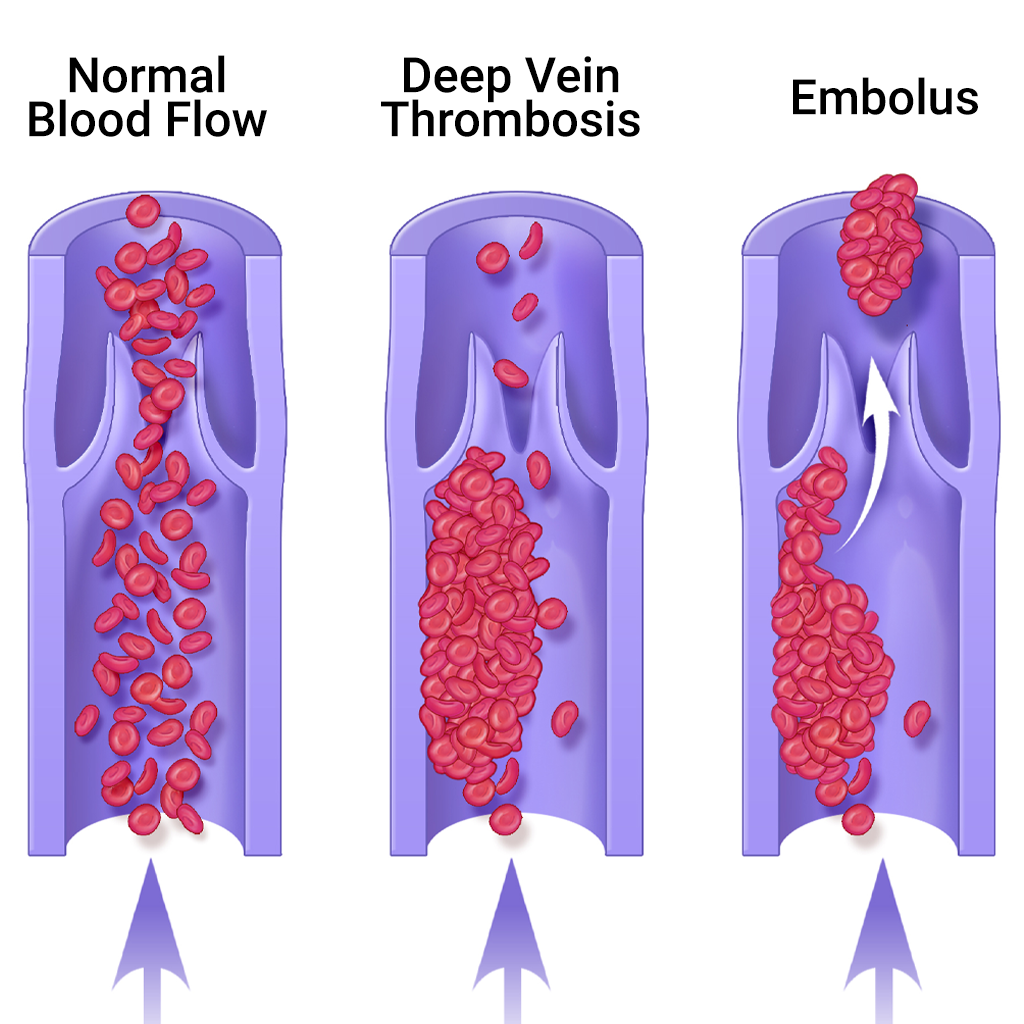
Post-thrombotic syndrome is an under-recognized, but relatively common after-effect of having DVT if treated with blood thinners alone, because the clot remains in the leg. Contrary to popular belief, anticoagulants do not actively dissolve the clot; they just prevent new clots from forming. While the body normally dissolves a clot over time, the vein can become damaged in the meantime.
Approximately half of these patients develop permanent, irreversible damage in the affected leg veins and their valves, resulting in abnormal pooling of blood in the leg, chronic leg pain, fatigue, swelling, and in extreme cases, severe skin ulcers. Many patients have to plan their daily activities around their legs, knowing that if they stand or exercise too long, their legs will swell or be painful.
Clot removal via a procedure called catheter-directed thrombolysis in selected cases of DVT can improve quality of life and prevent the debilitating effects of post-thrombotic syndrome.
How Is Deep Vein Thrombosis Treated at Memphis Vascular Center?
Catheter-directed thrombolysis is performed under imaging guidance by an interventional radiologist. It is designed to rapidly break up the clot, restore blood flow within the vein, and potentially preserve valve function to minimize the risk of post-thrombotic syndrome. The interventional radiologist inserts a catheter into the popliteal or other leg vein and threads it into the vein containing the clot using imaging guidance. The catheter tip is placed into the clot and a “clot-busting” drug is infused directly into the thrombus (clot). The fresher the clot, the faster it dissolves—one to two days. Early removal of the blood clots is likely to give patients their best chance to avoid disabling symptoms such as pain, swelling, and ulcer formation in the long run. Any narrowing in the vein that might lead to future clot formation can be identified by venography, an imaging study of the veins, and treated by the interventional radiologist with balloon angioplasty or stent placement.
In patients in whom this is not appropriate and blood thinners are contraindicated, an interventional radiologist can insert a vena cava filter, a small device that functions like a catcher’s mitt to capture blood clots but allows normal liquid blood to pass. People with symptoms of DVT should first go to an emergency room to seek help, to receive initial treatment with blood thinners to prevent a pulmonary embolism. After treatment with blood thinners, if symptoms such as leg pain and swelling continue, patients should consult with an interventional radiologist for further evaluation.